Researchers offer new treatment protocol for advanced head and neck cancer
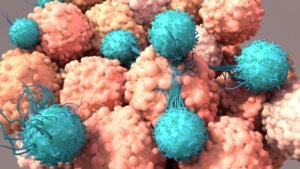
The current treatment of patients diagnosed with advanced or metastatic head and neck cancer (HNC) is ineffective. Ben-Gurion University of the Negev researchers, along with their international colleagues, have investigated and validated a potential treatment combination against the aggressive disease driven by hyper-activation of a specific signaling pathway, which is found in over 40% of HNC patients.
Their findings were just published in the Journal for ImmunoTherapy of Cancer.
Specifically, the authors showed in pre-clinical HNC models that treating tumor-bearing mice with a therapy that blocks this signaling pathway, sensitizes tumors to the immunotherapy of anti-PD1, resulting in the disappearance of tumors after the therapy combination. This effective treatment was validated in four HNC cancer models, and most mice were cured with no recurrent disease. Together with Dr. Pierre Saintygn from Lyon the authors also validated some of the findings in HNC patients.

The research was led by PhD student Manu Prasad in the laboratory of Prof. Moshe Elkabets in the Faculty of Health Sciences at Ben-Gurion University of the Negev.
“Our unique ability to generate pre-clinical HNC models and to investigate new treatment and treatment combinations provides hope for HNC patients. We sincerely hope that oncologists will test this treatment combination in HNC patients, as improving immunotherapy efficacy is crucial for prolonging the survival of cancer patients,” says Prof. Elkabets.
The authors also showed for the first time in mice bearing HNC that the treatment should be given sequentially. They found that a short treatment with trametinib is sufficient to sensitize anti-PD-1 resistant tumors. This sensitization happens because trametinib treatment, on the one hand, inhibits tumor cell proliferation and, on the other hand, down-regulates the expression of an immunosuppressive factor that determines the propagation of immunosuppressive cells in the tumor site. This effect enables cytotoxic white blood cells to reach the tumor site, and together with anti-PD1, can kill the tumor cells efficiently. However, when mice were treated with prolonged trametinib treatment, tumors failed to respond to immunotherapy.
The study was conducted by national and international groups from Soroka University Medical Center and Barzilai Medical Centers, Memorial Sloan Kettering, and Heidelberg Hospital.
####
This study was supported by the Cooperational Research Program of the Foundation Deutsches Krebsforschungszentrum, Heidelberg, with the Ministry of Science, Technology & Space (DKFZ-MOST #001192), the Israel Cancer Research Fund (ICRF 17-1693-RCDA), the United States — Israel Binational Science Foundation (BSF, 2017323), NSFC Israel-China project (#3409/20) and the Israel Science Foundation (ISF) Grant no. 700/16 and 302/21.
####
Journal Reference:
- Manu Prasad, Jonathan Zorea, Sankar Jagadeeshan, Avital B Shnerb, Sooraj Mathukkada, Jebrane Bouaoud, Lucas Michon, Ofra Novoplansky, Mai Badarni, Limor Cohen, Ksenia M Yegodayev, Sapir Tzadok, Barak Rotblat, Libor Brezina, Andreas Mock, Andy Karabajakian, Jérôme Fayette, Idan Cohen, Tomer Cooks, Irit Allon, Orr Dimitstein, Benzion Joshua, Dexin Kong, Elena Voronov, Maurizio Scaltriti, Yaron Carmi, Cristina Conde-Lopez, Jochen Hess, Ina Kurth, Luc G T Morris, Pierre Saintigny, Moshe Elkabets. MEK1/2 inhibition transiently alters the tumor immune microenvironment to enhance immunotherapy efficacy against head and neck cancer. Journal for ImmunoTherapy of Cancer, 2022; 10 (3): e003917 DOI: 10.1136/jitc-2021-003917